The Mpox outbreak in Africa serves as a stark reminder that diseases considered remote or minor in poorer regions can suddenly become major global threats. Historically, diseases like West Nile, Zika, and Chikungunya have followed similar patterns of neglect before emerging as significant concerns.
Mpox, initially discovered in monkeys in 1958 and in humans in 1970, was long viewed as a rare and localized infection in rural Africa. It wasn’t until a major outbreak in 2022 that it attracted substantial research funding, resulting in more studies in a year than in the previous six decades.
Calls from African researchers for increased global investment in Mpox prevention and treatment went largely unheeded until the recent surge. Now, with the WHO declaring the outbreak in central Africa a public health emergency of international concern, there’s a pressing need for a coordinated global response.
This situation highlights the global inequities in health resources, where vaccines and diagnostics are plentiful in wealthy countries but still scarce in much of Africa. It’s a reminder that no outbreak should be dismissed as “someone else’s problem,” as it can quickly become a worldwide issue.
The 2022 Mpox Outbreak: An Unexpected Global Challenge
The disease now known as “mpox” was formerly called “monkeypox” (MPXV) and is related to smallpox. Originally, it was considered a zoonotic infection mostly confined to central and west Africa, where it was transmitted mainly through contact with wild animals or bush meat. Human-to-human transmission was rare.
However, the dynamics changed dramatically in 2022. The outbreak evolved into a significant global issue, with over 99,000 confirmed cases reported in 116 countries. At its peak in August 2022, the number of new cases exceeded 6,000 per week.
This outbreak came as a surprise, particularly because it affected many non-endemic countries, with a notable incidence among men who have sex with men. Despite most cases being mild and the death toll around 200, the World Health Organization declared it a public health emergency of international concern on July 23, 2022.
The situation improved as the number of cases decreased, aided by behavioral changes and targeted vaccination campaigns. Vaccines and treatments, initially developed for potential bioterrorism scenarios, were distributed to many affected countries.
The outbreak involved clade II of MPXV, less virulent than clade I found in the Congo Basin. By May 2023, the emergency status was lifted, but while the worst appears to be over, the recent resurgence of cases highlights the need for ongoing vigilance.

Mpox Cases Surge in Africa
In 2023, Africa is experiencing a sharp rise in mpox cases. The continent, historically known for endemic mpox, is now encountering a mix of old and new challenges. Traditional zoonotic transmissions continue, while the effects of the 2022 global outbreak are evident, with new cases appearing in regions such as South Africa. Most concerning is the notable increase in MPXV clade Ib infections in the Democratic Republic of Congo, highlighting a troubling development in the region.
Emergence of a More Virulent Mpox Strain
The ongoing mpox outbreak is driven by clade I MPXV, formerly known as the Congo Basin strain, which is notably more severe than the clade II (West African) strain and comes with a higher fatality rate.
This outbreak is centered in South Kivu province in eastern DRC, where it has the potential to develop into a widespread pandemic. The strain exhibits a unique pattern of sustained human-to-human transmission, often through sexual contact, and its potential for increased transmissibility is still under investigation.
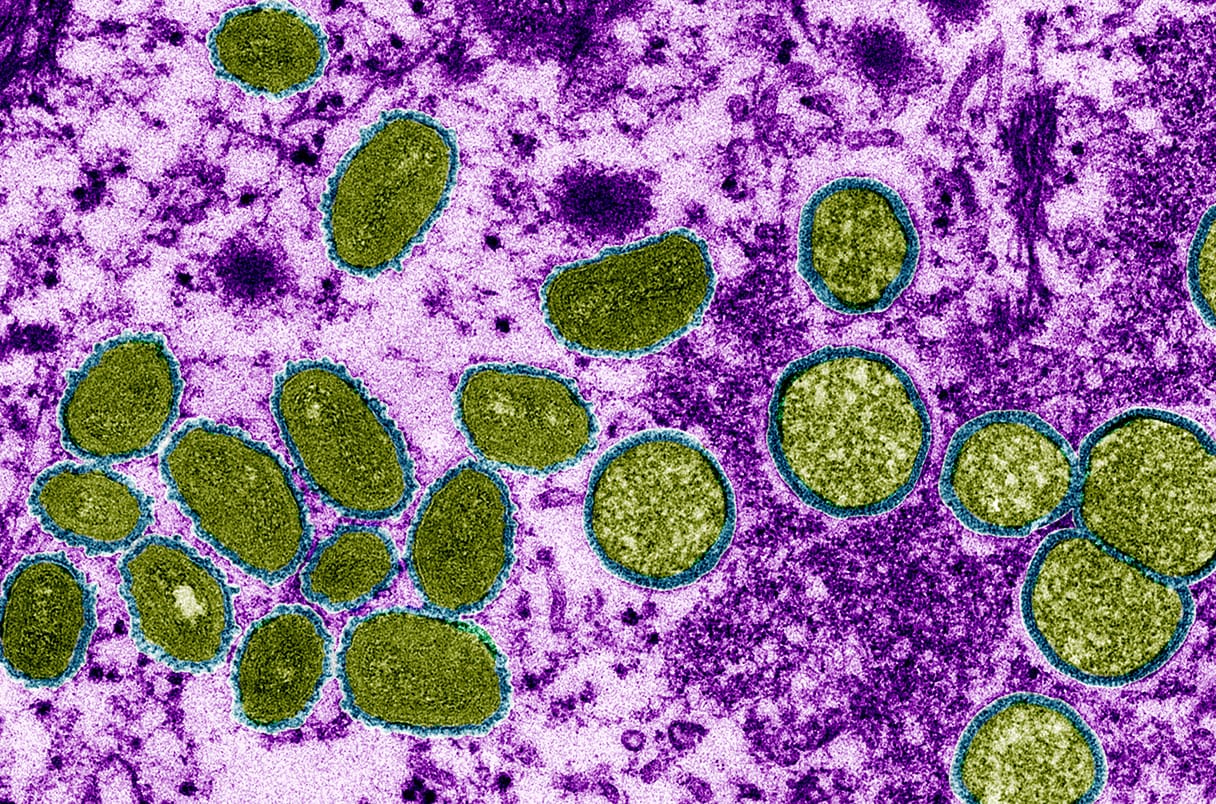
Clade Ib, the newly identified lineage causing the outbreak, has shown mutations typical of human-to-human spread, with this transmission likely starting around September 2023. Case numbers are rising rapidly, though many suspected cases may remain untested and unreported due to limitations in current diagnostic methods, which have not always detected this specific strain.
The strain primarily affects adults and has a higher fatality rate compared to the 2022 outbreak. It has already spread to several neighboring countries, including some like Kenya, which previously had no cases.
The situation is particularly challenging in eastern DRC, a region burdened by natural disasters, conflict, and other infectious diseases such as measles, cholera, and polio. The area has also recently experienced the second-largest Ebola outbreak, making the current crisis even more difficult to manage despite existing vaccines and treatments.
Key Actions to Combat the Mpox Outbreak
To effectively manage and contain the mpox outbreak and prevent it from growing into a larger epidemic or pandemic, several critical steps must be taken.
First, ensuring fair access to diagnostic tests, vaccines, and antiviral treatments is essential, which requires both strong political commitment and financial resources.

Ongoing scientific research is needed to understand how the disease spreads, the various exposure risks, and its clinical effects.
We propose forming an African-led, multi-disciplinary research group dedicated to studying and addressing mpox. This consortium would focus on developing strategies to eliminate mpox as a public health issue.
It’s vital for the global health community to recognize that localized outbreaks can quickly evolve into global threats, and to act decisively in response.